Omega-3 fatty acid
About this schools Wikipedia selection
SOS believes education gives a better chance in life to children in the developing world too. Click here for more information on SOS Children.
| Types of fats in food |
|---|
|
| See also |
|
Omega-3 fatty acids (also called ω−3 fatty acids or n−3 fatty acids) refers to a group of three fats called ALA (found in plant oils), EPA, and DHA (both commonly found in marine oils). Common sources of animal omega–3 EPA and DHA fatty acids include fish oils, algal oil, egg oil, squid oils, krill oil and some plant oils contain the omega 3 ALA fatty acid such as seabuckthorn seed and berry oils, flaxseed oil, Sacha Inchi oil, Echium oil, and hemp oil.
Omega-3 fatty acids are vital for normal metabolism but some of the potential health benefits of supplementation are controversial. Omega-3s are considered essential fatty acids, meaning that they cannot be synthesized by the human body -except that mammals have a limited ability, when the diet includes the shorter-chained omega-3 fatty acid ALA ( α-linolenic acid, 18 carbons and 3 double bonds), to form the more important long-chain omega−3 fatty acids, EPA ( eicosapentaenoic acid, 20 carbons and 5 double bonds) and then from EPA, the most crucial, DHA ( docosahexaenoic acid, 22 carbons and 6 double bonds) with even much greater inefficiency. The ability to make the longer-chained omega-3 fatty acids from ALA may also be impaired in aging. In foods exposed to air, unsaturated fatty acids are vulnerable to oxidation and rancidity. And fish are much more efficient than mammals at converting the ALA to the EPA and DHA omega−3 fatty acids.
Omega-3 fatty acids are polyunsaturated fatty acids with a double bond (C=C) at the third carbon atom from the end of the carbon chain. The fatty acids have two ends, the acid (-COOH) end, which is considered the beginning of the chain, thus "alpha", and the methyl (CH3) end, which is considered the "tail" of the chain, thus "omega." The nomenclature of the fatty acid is taken from the location of the first double bond, counted from the methyl end, that is, the omega (ω-) or the n- end.
Health effects
Supplementation does not appear to be associated with a lower risk of all-cause mortality.
Cancer
The evidence linking the consumption of fish to the risk of cancer is poor. Supplementation with omega-3 fatty acids does not appear to affect this risk either.
A 2006 report in the Journal of the American Medical Association, in their review of literature covering cohorts from many countries with a wide variety of demographics, concluded that there was no link between omega−3 fatty acids and cancer. This is similar to the findings of a review by the British Medical Journal of studies up to February 2002 that failed to find clear effects of long and shorter chain omega−3 fats on total mortality, combined cardiovascular events and cancer. In those with advanced cancer and cachexia, omega-3 fatty acids supplements may be of benefit, improving appetite, weight, and quality of life.
Cardiovascular disease
Evidence does not support a beneficial role for omega-3 fatty acid supplementation in preventing cardiovascular disease (including myocardial infarction and sudden cardiac death) or stroke. Fish oil supplementation has not been shown to benefit revascularization or arrythmia and has no effect on heart failure admission rates. Eating a diet high in fish that contain long chain omega-3 fatty acids does appear to decrease the risk of stroke.
Large amounts may increase low-density lipoproteins (LDL) (see below), up to 46%, although LDL changes from small to larger, buoyant, less atherogenic particles.
Omega-3 fatty acids also have mild antihypertensive effects. When subjects consumed omega-3 fatty acids from oily fish on a regular basis, their systolic blood pressure was lowered by about 3.5–5.5 mmHg. The 18 carbon α-linolenic acid (ALA) has not been shown to have the same cardiovascular benefits that DHA or EPA may have.
Some evidence suggests that people with certain circulatory problems, such as varicose veins, may benefit from the consumption of EPA and DHA, which may stimulate blood circulation, increase the breakdown of fibrin, a compound involved in clot and scar formation, and, in addition, may reduce blood pressure. Evidently, omega−3 fatty acids reduce blood triglyceride levels, and regular intake may reduce the risk of secondary and primary heart attack. ALA does not confer the cardiovascular health benefits of EPA and DHA.
Large amounts may increase the risk of hemorrhagic stroke (see below); lower amounts are not related to this risk; 3 grams of total EPA/DHA daily are generally recognized as safe (GRAS) with no increased risk of bleeding involved and many studies used substantially higher doses without major side effects (for example: 4.4 grams EPA/2.2 grams DHA in 2003 study).
Among omega-3 fatty acids, neither long-chain nor short-chain forms were consistently associated with breast cancer risk. High levels of docosahexaenoic acid (DHA), however, the most abundant omega-3 PUFA in erythrocyte ( red blood cell) membranes, were associated with a reduced risk of breast cancer. The DHA obtained through the consumption of polyunsaturated fatty acids is positively associated with cognitive and behavioural performance. In addition DHA is vital for the grey matter structure of the human brain, as well as retinal stimulation and neurotransmission.
Inflammation
Although not confirmed as an approved health claim, current research suggests that the anti-inflammatory activity of long-chain omega−3 fatty acids may translate into clinical effects. For example, there is evidence that rheumatoid arthritis sufferers taking long-chain omega−3 fatty acids from sources such as fish have reduced pain compared to those receiving standard NSAIDs. Some potential benefits have been reported in conditions such as rheumatoid arthritis.
Developmental disorders
Although not supported by current scientific evidence as a primary treatment for ADHD, autism spectrum disorders, and other developmental differences, omega-3 fatty acids have gained popularity for children with these conditions.
Omega-3 fatty acids offer a promising complementary approach to standard treatments for ADHD and developmental coordination disorder. Fish oils appear to reduce ADHD-related symptoms in some children. A randomized, controlled trial has suggested that "fatty acid supplementation may offer a safe efficacious treatment option for educational and behavioural problems among children with DCD" .
There is not enough scientific evidence to support the effectiveness of omega-3 fatty acids for autism spectrum disorders.
Fish oil has only a small benefit on the risk of early birth.
Psychiatric disorders
Though there is some evidence that omega-3 fatty acids are related to a variety of mental disorders, they may tentatively be useful as an add-on for the treatment of depression associated with bipolar disorder and there is preliminary evidence that EPA supplementation is helpful in cases of depression. There is, however, a significant risk of bias in the literature.
Cognitive aging
Epidemiological studies suggest that consumption of omega-3 fatty acids can reduce the risk of dementia, but evidence of a treatment effect in dementia patients is inconclusive. However, clinical evidence suggests benefits of treatment specifically in patients who show signs of cognitive decline but who are not sufficiently impaired to meet criteria for dementia.
Adverse effects
In a letter published October 31, 2000, the United States Food and Drug Administration Centre for Food Safety and Applied Nutrition, Office of Nutritional Products, Labeling, and Dietary Supplements noted that known or suspected risks of EPA and DHA consumed in excess of 3 grams per day may include the possibility of:
- Increased incidence of bleeding
- Hemorrhagic stroke
- Oxidation of omega-3 fatty acids, forming biologically active oxidation products
- Increased levels of low-density lipoproteins (LDL) cholesterol or apoproteins associated with LDL cholesterol among diabetics and hyperlipidemics
- Reduced glycemic control among diabetics
Chemistry
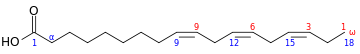
Omega−3 fatty acids that are important in human physiology are α-linolenic acid (18:3, n−3; ALA), eicosapentaenoic acid (20:5, n−3; EPA), and docosahexaenoic acid (22:6, n−3; DHA). These three polyunsaturates have either 3, 5, or 6 double bonds in a carbon chain of 18, 20, or 22 carbon atoms, respectively. As with most naturally-produced fatty acids, all double bonds are in the cis-configuration, in other words, the two hydrogen atoms are on the same side of the double bond; and the double bonds are interrupted by methylene bridges (-CH
2-), so that there are two single bonds between each pair of adjacent double bonds.
List of omega−3 fatty acids
This table lists several different names for the most common omega−3 fatty acids found in nature.
| Common name | Lipid name | Chemical name |
|---|---|---|
| Hexadecatrienoic acid (HTA) | 16:3 (n−3) | all-cis-7,10,13-hexadecatrienoic acid |
| α-Linolenic acid (ALA) | 18:3 (n−3) | all-cis-9,12,15-octadecatrienoic acid |
| Stearidonic acid (SDA) | 18:4 (n−3) | all-cis-6,9,12,15-octadecatetraenoic acid |
| Eicosatrienoic acid (ETE) | 20:3 (n−3) | all-cis-11,14,17-eicosatrienoic acid |
| Eicosatetraenoic acid (ETA) | 20:4 (n−3) | all-cis-8,11,14,17-eicosatetraenoic acid |
| Eicosapentaenoic acid (EPA) | 20:5 (n−3) | all-cis-5,8,11,14,17-eicosapentaenoic acid |
| Heneicosapentaenoic acid (HPA) | 21:5 (n−3) | all-cis-6,9,12,15,18-heneicosapentaenoic acid |
| Docosapentaenoic acid (DPA), Clupanodonic acid |
22:5 (n−3) | all-cis-7,10,13,16,19-docosapentaenoic acid |
| Docosahexaenoic acid (DHA) | 22:6 (n−3) | all-cis-4,7,10,13,16,19-docosahexaenoic acid |
| Tetracosapentaenoic acid | 24:5 (n−3) | all-cis-9,12,15,18,21-tetracosapentaenoic acid |
| Tetracosahexaenoic acid (Nisinic acid) | 24:6 (n−3) | all-cis-6,9,12,15,18,21-tetracosahexaenoic acid |
Mechanism of action
The 'essential' fatty acids were given their name when researchers found that they are essential to normal growth in young children and animals, though the modern definition of ' essential' is stricter. A small amount of omega−3 in the diet (~1% of total calories) enabled normal growth, and increasing the amount had little to no additional effect on growth.
Likewise, researchers found that omega-6 fatty acids (such as γ-linolenic acid and arachidonic acid) play a similar role in normal growth. However, they also found that omega−6 was "better" at supporting dermal integrity, renal function, and parturition. These preliminary findings led researchers to concentrate their studies on omega−6, and it is only in recent decades that omega−3 has become of interest.
In 1964, it was discovered that enzymes found in sheep tissues convert omega−6 arachidonic acid into the inflammatory agent called prostaglandin E2, which both causes the sensation of pain and expedites healing and immune response in traumatized and infected tissues. By 1979, more of what are now known as eicosanoids were discovered: thromboxanes, prostacyclins, and the leukotrienes. The eicosanoids, which have important biological functions, typically have a short active lifetime in the body, starting with synthesis from fatty acids and ending with metabolism by enzymes. However, if the rate of synthesis exceeds the rate of metabolism, the excess eicosanoids may have deleterious effects. Researchers found that certain omega−3 fatty acids are also converted into eicosanoids, but at a much slower rate. Eicosanoids made from omega−3 fatty acids are often referred to as anti-inflammatory, but in fact they are just less inflammatory than those made from omega−6 fats. If both omega−3 and omega−6 fatty acids are present, they will "compete" to be transformed, so the ratio of long-chain omega−3:omega−6 fatty acids directly affects the type of eicosanoids that are produced.
This competition was recognized as important when it was found that thromboxane is a factor in the clumping of platelets, which can both cause death by thrombosis and prevent death by bleeding. Likewise, the leukotrienes were found to be important in immune/inflammatory-system response, and therefore relevant to arthritis, lupus, asthma, and recovery from infections. These discoveries led to greater interest in finding ways to control the synthesis of omega−6 eicosanoids. The simplest way would be by consuming more omega−3 and fewer omega−6 fatty acids.
They are required during the prenatal period for the formation of synapses and cell membranes. These processes are also essential in postnatal human development for injury response of the central nervous system and retinal stimulation.
Interconversion
Conversion efficiency of ALA to EPA and DHA
The body converts short-chain omega−3 fatty acids to long-chain forms (EPA, DHA) with an efficiency below 5% in men. The omega-3 conversion efficiency is greater in women, possibly because of the importance for meeting the demands of the fetus and neonate for DHA.
These conversions occur competitively with omega−6 fatty acids, which are essential closely related chemical analogues that are derived from linoleic acid. Both the omega−3 α-linolenic acid and omega−6 linoleic acid must be obtained from food. Synthesis of the longer omega−3 fatty acids from linolenic acid within the body is competitively slowed by the omega−6 analogues. Thus, accumulation of long-chain omega−3 fatty acids in tissues is more effective when they are obtained directly from food or when competing amounts of omega−6 analogs do not greatly exceed the amounts of omega−3.
The conversion of ALA to EPA and further to DHA in humans has been reported to be limited, but varies with individuals. Women have higher ALA conversion efficiency than men, which is presumed to be due to the lower rate of use of dietary ALA for beta-oxidation. This suggests that biological engineering of ALA conversion efficiency is possible. Goyens et al. argue that it is the absolute amount of ALA, rather than the ratio of omega−3 and omega−6 fatty acids, that controls the conversion efficiency.
The omega−6 to omega−3 ratio
Some older clinical studies indicate that the ingested ratio of omega−6 to omega−3 (especially linoleic vs alpha-linolenic) fatty acids is important to maintaining cardiovascular health. However, three studies published in 2005, 2007 and 2008, including a randomized controlled trial, found that while omega−3 polyunsaturated fatty acids are extremely beneficial in preventing heart disease in humans, the levels of omega−6 polyunsaturated fatty acids (and therefore the ratios) were insignificant.
Both omega−6 and omega−3 fatty acids are essential; i.e., humans must consume them in the diets. Omega−6 and omega−3 eighteen-carbon polyunsaturated fatty acids compete for the same metabolic enzymes, thus the omega−6:omega−3 ratio of ingested fatty acids has significant influence on the ratio and rate of production of eicosanoids, a group of hormones intimately involved in the body's inflammatory and homeostatic processes which includes the prostaglandins, leukotrienes, and thromboxanes, among others. Altering this ratio can change the body's metabolic and inflammatory state. In general, grass-fed animals accumulate more omega−3 than do grain-fed animals, which accumulate relatively more omega−6. Metabolites of omega−6 are more inflammatory (esp. arachidonic acid) than those of omega−3. This necessitates that omega−6 and omega−3 be consumed in a balanced proportion; healthy ratios of omega−6:omega−3, according to some authors, range from 1:1 to 1:4 (an individual needs more omega−3 than omega−6). Other authors believe that ratio 4:1 (when the amount of omega-6 is only 4 times greater than that of omega-3) is already healthy. Studies suggest the evolutionary human diet, rich in game animals, seafood, and other sources of omega−3, may have provided such a ratio.
Typical Western diets provide ratios of between 10:1 and 30:1 (i.e., dramatically higher levels of omega−6 than omega-3). The ratios of omega−6 to omega−3 fatty acids in some common vegetable oils are: canola 2:1, hemp 2-3:1, soybean 7:1, olive 3–13:1, sunflower (no omega−3), flax 1:3, cottonseed (almost no omega−3), peanut (no omega−3), grapeseed oil (almost no omega−3) and corn oil 46:1 ratio of omega−6 to omega−3.
History
Although omega-3 fatty acids have been known as essential to normal growth and health since the 1930s, awareness of their health benefits has dramatically increased since the 1990s.
The health benefits of the long-chain omega-3 fatty acids — primarily EPA and DHA are the best known. These benefits were discovered in the 1970s by researchers studying the Greenland Inuit Tribe. The Greenland Inuit people consumed large amounts of fat from fish, but displayed virtually no cardiovascular disease. The high level of omega-3 fatty acids consumed by the Inuit reduced triglycerides, heart rate, blood pressure, and atherosclerosis.
On September 8, 2004, the U.S. Food and Drug Administration gave "qualified health claim" status to EPA and DHA omega−3 fatty acids, stating, "supportive but not conclusive research shows that consumption of EPA and DHA [omega−3] fatty acids may reduce the risk of coronary heart disease." This updated and modified their health risk advice letter of 2001 (see below). As of this writing, regulatory agencies do not accept that there is sufficient evidence for any of the suggested benefits of DHA and EPA other than for cardiovascular health, and further claims should be treated with caution.
The Canadian Government has recognized the importance of DHA omega-3 and permits the following biological role claim for DHA: "DHA, an omega-3 fatty acid, supports the normal development of the brain, eyes and nerves."