Measles
About this schools Wikipedia selection
SOS Children have produced a selection of wikipedia articles for schools since 2005. Do you want to know about sponsoring? See www.sponsorachild.org.uk
| Measles | |
|---|---|
| Classification and external resources | |
 Skin of a patient after 3 days of measles infection. |
|
| ICD- 10 | B 05.- |
| ICD- 9 | 055 |
| DiseasesDB | 7890 |
| MedlinePlus | 001569 |
| eMedicine | derm/259 ped/1388 |
| Measles virus | |
|---|---|
 |
|
| Measles virus | |
| Virus classification | |
| Group: | Group V ( (-)ssRNA) |
| Order: | Mononegavirales |
| Family: | Paramyxoviridae |
| Genus: | Morbillivirus |
| Type species | |
| Measles virus |
|
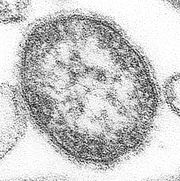
Measles, also known as 'rougeole' in French, is a disease caused by a virus, specifically a paramyxovirus of the genus Morbillivirus. 'German measles' is an unrelated condition caused by the rubella virus.
Measles is spread through respiration (contact with fluids from an infected person's nose and mouth, either directly or through aerosol transmission), and is highly contagious—90% of people without immunity sharing a house with an infected person will catch it. Airborne precautions should be taken for all suspected cases of measles.
The incubation period usually lasts for 4–12 days (during which there are no symptoms). Infected people remain contagious from the appearance of the first symptoms until 3–5 days after the rash appears.
Reports of measles go as far back to at least 600 B.C. however, the first scientific description of the disease and its distinction from smallpox is attributed to the Persian physician Ibn Razi (Rhazes) 860-932 who published a book entitled "The Book of Smallpox and Measles" (in Arabic: Kitab fi al-jadari wa-al-hasbah). In roughly the last 150 years, measles has been estimated to have killed about 200 million people worldwide. In 1954, the virus causing the disease was isolated from an 11-year old boy from the US, David Edmonston, and adapted and propagated on chick embryo tissue culture. To date, 21 strains of the measles virus have been identified. Licensed vaccines to prevent the disease became available in 1963.
Symptoms
The classical symptoms of measles include a fever for at least three days, the three Cs— cough, coryza (runny nose) and conjunctivitis (red eyes). The fever may reach up to 40° Celsius (104° Fahrenheit). Koplik's spots seen inside the mouth are pathognomonic (diagnostic) for measles but are not often seen, even in real cases of measles, because they are transient and may disappear within a day of arising.
The characteristic measles rash is classically described as a generalized, maculopapular, erythematous rash that begins several days after the fever starts. It starts on the head before spreading to cover most of the body, often causing itching. The rash is said to "stain", changing colour from red to dark brown, before disappearing.
Diagnosis and treatment
Clinical diagnosis of measles requires a history of fever of at least three days together with at least one of the three Cs. Observation of Koplik's spots is also diagnostic of measles.
Alternatively, laboratory diagnosis of measles can be done with confirmation of positive measles IgM antibodies or isolation of measles virus RNA from respiratory specimens. In cases of measles infection following secondary vaccine failure IgM antibody may not be present. In these cases serological confirmation may be made by showing IgG antibody rises by Enzyme immunoasay or complement fixation. In children, where phlebotomy is inappropriate, saliva can be collected for salivary measles specific IgA test.
Positive contact with other patients known to have measles adds strong epidemiological evidence to the diagnosis.
There is no specific treatment or antiviral therapy for uncomplicated measles. Most patients with uncomplicated measles will recover with rest and supportive treatment.
Some patients will develop pneumonia as a sequela to the measles. Histologically, a unique cell can be found in the paracortical region of hyperplastic lymph nodes in patients affected with this condition. This cell, known as the Warthin-Finkeldey cell, is a multinucleated giant with eosinophilic cytoplasmic and nuclear inclusions.
Transmission
The measles is a highly contagious airborne pathogen which spreads primarily via the respiratory system. The virus is transmitted in respiratory secretions, and can be passed from person to person via aerosol droplets containing virus particles, such as those produced by a coughing patient. Once transmission occurs, the virus infects and replicates in the lymphatic system, urinary tract, conjunctivae, blood vessels and central nervous system of its new host. The role of epithelial cells is uncertain, but the virus must infect them to spread to a new individual.
Patients with the measles should be placed on droplet precautions.
Humans are the only known natural hosts of measles, although the virus can infect some non-human primate species.
Complications
Complications with measles are relatively common, ranging from relatively mild and less serious diarrhea, to pneumonia and encephalitis ( subacute sclerosing panencephalitis), corneal ulceration leading to corneal scarring Complications are usually more severe amongst adults who catch the virus.
The fatality rate from measles for otherwise healthy people in developed countries is low: approximately 1 death per thousand cases. In underdeveloped nations with high rates of malnutrition and poor healthcare, fatality rates of 10 percent are common. In immunocompromised patients, the fatality rate is approximately 30 percent.
Public health
Measles is a significant infectious disease because, while the rate of complications is not high, the disease itself is so infectious that the sheer number of people who would suffer complications in an outbreak amongst non-immune people would quickly overwhelm available hospital resources. If vaccination rates fall, the number of non-immune persons in the community rises, and the risk of an outbreak of measles consequently rises.
In developed countries, most children are immunized against measles by the age of 18 months, generally as part of a three-part MMR vaccine (measles, mumps, and rubella). The vaccination is generally not given earlier than this because children younger than 18 months usually retain anti-measles immunoglobulins (antibodies) transmitted from the mother during pregnancy. A "booster" vaccine is then given between the ages of four and five. Vaccination rates have been high enough to make measles relatively uncommon. Even a single case in a college dormitory or similar setting is often met with a local vaccination program, in case any of the people exposed are not already immune. In developing countries, measles remains common.
Unvaccinated populations are at risk for the disease. After vaccination rates dropped in northern Nigeria in the early 2000s due to religious and political objections, the number of cases rose significantly, and hundreds of children died. A 2005 measles outbreak in Indiana was attributed to children whose parents refused vaccination. In the early 2000s the MMR vaccine controversy in the United Kingdom regarding a potential link between the combined MMR vaccine (vaccinating children from mumps, measles and rubella) and autism prompted a comeback in the measles party, where parents deliberately infect the child with measles to build up the child's immunity without an injection. This practice poses many health risks to the child, and has been discouraged by the public health authorities. Scientific evidence provides no support for the hypothesis that MMR plays a role in causing autism. However, the MMR scare in Britain caused uptake of the vaccine to plunge, and measles cases came back: 2007 saw 971 cases in England and Wales, the biggest rise in occurrence in measles cases since records began in 1995.
According to the World Health Organization (WHO), measles is a leading cause of vaccine preventable childhood mortality. Worldwide, the fatality rate has been significantly reduced by partners in the Measles Initiative: the American Red Cross, the United States Centers for Disease Control and Prevention (CDC), the United Nations Foundation, UNICEF and the World Health Organization (WHO). Globally, measles deaths are down 60 percent, from an estimated 873,000 deaths in 1999 to 345,000 in 2005. Africa has seen the most success, with annual measles deaths falling by 75 percent in just 5 years, from an estimated 506,000 to 126,000.
The joint press release by members of the Measles Initiative brings to light another benefit of the fight against measles: "Measles vaccination campaigns are contributing to the reduction of child deaths from other causes. They have become a channel for the delivery of other life-saving interventions, such as bed nets to protect against malaria, de-worming medicine and vitamin A supplements. Combining measles immunization with other health interventions is a contribution to the achievement of Millennium Development Goal Number 4: a two-thirds reduction in child deaths between 1990 and 2015."
Recent outbreaks
In 2007, a large measles outbreak in Japan caused a number of universities and other institutions to close in an attempt to contain the disease.
Approximately 1000 cases of the disease were reported in Israel between August 2007 and May 2008 (in sharp contrast to just some dozen cases the year before). Many children in ultra-Orthodox Jewish communities were affected due to low vaccination coverage. As of 2008 the disease is endemic in the United Kingdom and epidemics have been reported in Austria, Italy and Switzerland. Low vacciation rates are responsible.
United States
Indigenous measles were declared to have been eliminated in North, Central, and South America; the last endemic case in the region was reported on November 12, 2002. Outbreaks are still occurring, however, following importations of measles viruses from other world regions. In June 2006, an outbreak in Boston resulted after a resident became infected in India, and in October 2007, a Michigan girl who had been vaccinated contracted the disease overseas.
Between January 1 and April 25, 2008, a total of 64 confirmed measles cases were preliminarily reported in the United States to the Centers for Disease Control and Prevention, the most reported by this date for any year since 2001. Of the 64 cases, 54 were associated with importation of measles from other countries into the United States, and 63 of the 64 patients were unvaccinated or had unknown or undocumented vaccination status.
By July 9, 2008, a total of 127 cases were reported in 15 states (including 22 in Arizona), making it the largest US outbreak since 1997 (when 138 cases were reported). Most of the cases were acquired outside of the United States and afflicted individuals who had not been vaccinated.